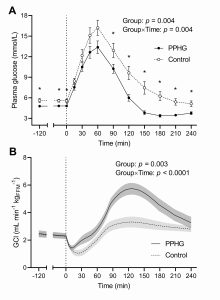
Background: Postprandial hypoglycemia (PPHG) is an underrecognized complication of gastric bypass in people with type 2 diabetes (T2D), whose mechanisms remain unclear. Using an integrated physiology approach, we examined the prevalence of post-bypass PPHG and dissected its pathophysiological determinants in T2D. Materials and methods: In this case-control study, subjects with history of T2D treated with Roux-en-Y gastric bypass (RYGB) 1-4 years before enrollment underwent a dual-labeled, 300-min, 75g oral glucose tolerance test (OGTT). Plasma glucose, glucose tracers, insulin, C peptide, GLP-1, GIP, glucagon, epinephrine, norepinephrine, and cortisol were measured. PPHG was defined as a plasma glucose nadir <3.0 mmol/L without symptoms or <3.3 mmol/L with symptoms of hypoglycemia. Mathematical models were implemented to estimate glucose metabolic fluxes and β-cell function parameters. Repeated ECG and blood pressure measurements were used to detect counterregulatory sympathetic activation. Results: A total of 24 subjects completed the assessments (14 women, age 54±9 years, BMI 29.3±6.3 kg/m2, HbA1c 36±6 mmol/mol). PPHG occurred in 12 (50%) subjects (Panel A). Compared with those without hypoglycemia, PPHG subjects were more frequently women and had better glycemic control, with a greater rate of diabetes remission (100% vs 58%, p=0.04), despite similar age and body mass. PPHG was associated with higher tracer-derived glucose clearance (Panel B) due to early glucose-stimulated hyperinsulinemia and higher insulin sensitivity. Hyperinsulinemia was driven by enhanced β-cell function and reduced insulin clearance, while incretin hormones were similar between groups. PPHG subjects also had inadequate counterregulatory hormone responses to hypoglycemia, preventing the physiological compensatory increase in endogenous glucose production. The independent effect of glucose clearance on PPHG was confirmed in multivariable analysis and after excluding subjects with post-surgery diabetes relapse. Cardiovascular and hemodynamic parameters were unaffected by hypoglycemia. Conclusion: PPHG frequently occurs in patients with T2D remission after gastric bypass driven by excessive glucose clearance due to early hyperinsulinemia and high insulin sensitivity, while defective counterregulation hinders the compensatory increase in glucose production. Post-bypass PPHG should be actively searched in T2D for its potential negative health consequences.