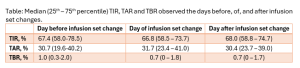
Background: Subjects with type 1 diabetes (T1D) using Advanced Hybrid Closed Loop Systems (AHCLS) show better glycemic control than those using other types of continuous subcutaneous insulin infusion systems. Infusion set change may impact on glucose control in patients on CSII. Whether set change influences glucose control in patients using AHCLS is not clear. Aim: To evaluate glycemic variations occurring in occasion of set changes in people with T1D treated with AHCLS. Methods: Eighty subjects using AHCLS were consecutively enrolled. Data about time in range (TIR), time above range (TAR), and time below range (TBR) registered before (day -1), after (day +1) and on (day 0) the days of all set changes occurring during the 14 days before enrollment were collected. Clinical features (age, sex, disease duration, body mass index [BMI], HbA1c, duration of pump therapy and set duration) were also retrieved. Results: During the 14 days evaluated in this analysis, patients changed the infusion set 2.9±0.7 times. Overall mean TIR, TAR or TBR of days 0 and days +1 were similar to days -1 (Tab.), with no differences among different AHCLS. However, a wide variability among study participants in the difference of mean TIR between days 0 and days -1 (Δ0, -1 TIR) was observed (mean Δ0, -1 TIR -1.6%±11.9%). Therefore, we investigated for factors associated with Δ0, -1 TIR. After multivariate regression analyses accounting for confounders, we found that only BMI (β for (ln)BMI +15.7, p=0.030) and mean TIR on day -1 (β -0.46, p<0.001) were significantly related to Δ0, -1 TIR. Specifically, subjects with BMI<23 kg/m2 showed a significant worsening of TIR compared to those with BMI≥23 kg/m2 (-6.3±8.6% vs +0.8± 12.7%, p=0.011), mainly driven by an increase in TBR (% of patients experiencing an increase in TBR: 48.2% vs 28.3%, among those with BMI<23 and ≥23 kg/m2, respectively, p=0.078). Conclusions: Infusion set change does not impact on glycemic control in patients on AHCLS, but we observed that there is an important variability among subjects. Such variability appears mainly associated with differences in BMI, with leaner patients being at higher risk of TIR and TBR worsening during the day of set change.