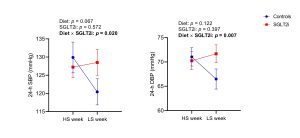
Background: Animal studies have shown that sodium glucose cotransporter-2 inhibitors (SGLT2i) blunt the hypertensive response to a sodium load, possibly contributing to their cardiorenal benefits. We explored the effects of SGLT2i on the sensitivity of BP to dietary sodium intake (salt-sensitivity) in patients with type 2 diabetes (T2D), and the underlying physiological mechanisms. Methods: We conducted a case-control trial on 21 patients with non-insulin dependent T2D divided into SGLT2i-treated patients (n=9) and those treated with other anti-diabetic drugs (n=12). Participants underwent a cross-over dietary intervention consisting of a week of high-sodium diet (HS week, 4.800 mg/day) followed by a week of low-sodium diet (LS week, 1.200 mg/day). The primary endpoint was salt-sensitivity of BP, defined as the between-week change in systolic (SBP) and diastolic BP (DBP), measured through 24-h ambulatory BP monitoring (24-h ABPM). Secondary endpoints included post-feeding natriuresis after a standardized meal, and between-week changes in extracellular to total body water ratio (ECW/TBW, bioimpedance-measured) and plasma renin and aldosterone (neuro-hormonal activation). Results: The two groups had comparable baseline characteristics (whole population: age 66±8 years, M/F [%] 71/29, BMI 28±3 kg/m2, HbA1c 51±7 mmol/mol, SBP/DBP 140±13/ 81±10 mmHg, eGFR 81±14 ml/min/1.73m2). SGLT2i treatment reduced the effect of sodium intake on 24-h SBP (pint=0.020) and DBP (pint=0.007), with smaller changes between LS and HS-week compared to controls (ΔSBP24h: +1.3±9.0 vs -7.8±10.3 mmHg, p=0.026; ΔDBP24h: +1.4±4.8 vs -3.5±4.8 mmHg, p=0.012). Consistently, SGLT2i-treated patients also showed a reduced effect of sodium intake on day-time SBP (pint=0.012) and DBP (pint=0.024) and night-time DBP (pint=0.037). Additionally, SGLT2i-treated patients tended to show lower neuro-hormonal activation in response to sodium deprivation compared to controls (reninLS-HS +21±87 vs +249±429 mUI/l, p=0.060; aldosteroneLS-HS +0.9±5.4 vs +3.5±4.6 ng/dl, p=0.138), while changes in hydration status and post-feeding natriuresis were comparable between groups. Conclusion: SGLT2i-treated patients display a reduced salt-sensitivity of BP and numerically blunted neuro-hormonal activation in response to dietary sodium changes. These effects may contribute to the established cardiorenal benefits of SGLT2i treatment. Funded by Fondazione Diabete Ricerca SID; EFSD Lilly Young Investigator Research Award.