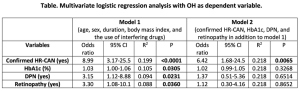
Objectives: The study investigates determinants of orthostatic hypotension (OH) in type 1 diabetes (T1D), and the usefulness of a new index of cardiac baroreflex function to discriminate neurogenic from non-neurogenic OH. Methods: In 124 participants with T1D [age 41.4±12.3, duration 22.0 (IQR 14.0-31.5) years], we performed 3 heart rate based cardiovascular reflex tests (HR-CARTs) and OH test and assessed diabetic polyneuropathy (DPN), clinical history and variables. We defined OH as a systolic blood pressure fall (∆SBP) ≥20 and ≥30 mmHg in presence of supine SBP<140 and ≥140 mmHg, respectively, and confirmed cardiovascular autonomic neuropathy (HR-CAN) with 2 abnormal HR-CARTs. We used the change in HR by the fall in SBP after standing (ΔHR/ΔSBP ratio) to classify OH as neurogenic or not according to a value <0.5 or >0.5 bpm/mmHg. Results: OH was present in 25 participants, including 9 with normal HR-CARTs, and was associated with lower HR-CARTs (deep breathing: p=0.0003; lying to standing: p<0.0001; Valsalva manoeuvre: p=0.0368), with higher scores of neuropathic symptoms (p=0.0034) and signs (p=0.0433), with higher HbA1c (p=0.0027), with confirmed HR-CAN (p<0.0001) and DPN (p=0.0074). Table shows the determinants of OH. ∆SBP had good diagnostic accuracy for confirmed HR-CAN [area under the curve (AUC): 0.79±0.06 (95%CI 0.68-0.90); sensitivity: 50%; specificity: 87%]. When excluding the use of interfering drugs, AUC increased to 0.82±0.06, sensitivity to 58% and specificity to 91%. AUC of ΔHR/ΔSBP in discriminating among participants with OH those with (neurogenic OH) and without confirmed HR-CAN (non-neurogenic OH), was 0.72±0.11 (0.51-0.92), with sensitivity of 67% and specificity of 61%, and increased to 0.86±0.09 when excluding interfering drugs, with sensitivity of 67% and specificity of 100%. Conclusions: CAN is the main independent determinant of OH in people with T1D and OH keeps a high specificity for confirmed CAN. The ΔHR/ΔSBP has a fair diagnostic accuracy for neurogenic OH, although less than described in non-diabetic population. The utility of this index, easily achievable in the clinical setting, deserves to be further investigated in diabetes.