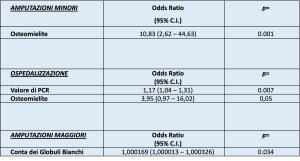
Background: The characteristic lesions of the diabetic foot are chronic ulcers, in addition to pre-ulcerative and post-ulcerative lesions and infectious complications. Diabetic foot complicated by infection is the most frequent cause of hospitalization among subjects with diabetes mellitus and the main determinant of amputations in these patients. Methods: A retrospective, observational, single-center study was carried out on a cohort of 56 patients belonging to the UOC of Internal Medicine IGR of the ARNAS Civico Di Cristina Benfratelli in Palermo. Based on clinical, diagnostic and instrumental needs, patients were treated as outpatient or as inpatient. Adult patients with a confirmed diagnosis of Diabetic Foot complicated by moderate or severe infection (according to IWGDF 2023 guidelines) were enrolled. The minimal duration of follow-up after the enrollment was 6 months. The primary outcomes assessed are: healing at six months, amputations (major and minor) and hospitalization. We made the comparison between the two groups (moderate infection VS severe infection) in relation to the four primary outcomes chosen. Results: In the observation period from June 2022 to June 2023, a total of 56 patients were enrolled. White blood cell counts were statistically significant in the comparison between the two groups: 10.68 (9.71-11.50 x 10³/uL) in moderately infected patients vs 15.24 (13.28-17.20 x 10³/uL) in severely infected patients. (p value=0.003). The C-Reactive Protein (normal values <0.5 mg/dL) was significantly higher: 17.4 (14.6-20.2 mg/dL) in the severely infected group vs 6.1 (3.5-8.6 mg/dL) in moderately infected patients. All patients in the severely infected group were hospitalized, while 39.32% of patients with moderate infection required hospitalization. There were no statistically significant differences in the rate of major amputations and the six-month healing rate. In contrast, the rate of minor amputation was significantly higher in patients belonging to the group of severe infections. (67.8% vs 37.7%; p=0.003). In the multivariate analysis performed, the presence of osteomyelitis at the time of diagnosis increases the risk of minor amputation (odds ratio 10.83; p<0.001) by more than ten times compared to subjects without osteomyelitis. Conclusions: the presence of osteomyelitis in one of the main predictor of unfavorable outcome as it is related to a higher rate of hospitalization and minor amputation.