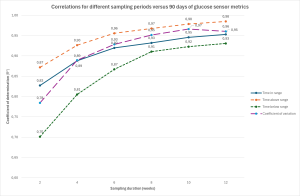
Aims: According to the 2023 International Consensus, 14 days of glucose sensor data strongly correlate with 90 days data for time in range 70-180 mg/dl (TIR) and above range (TAR), but longer sampling periods might be needed for the evaluation of the relationship for time below range (TBR) and coefficient of variation (CV). Aim of this real-life retrospective study is to provide updated information about the strength of the correlations of different sampling periods versus 90 days for all glucose metrics. Methods: All subjects with type 1 diabetes (T1D) in multiple insulin injection therapy, with flash glucose monitoring (FGM) use ≥70% over the 3 months prior to visits, were consecutively recruited at Verona Diabetes Center between January and December 2023. For all glucose metrics, correlations were computed for 3-month intervals versus selected shorter sampling periods from 2 to 12 weeks, and coefficients of determination (R2) were assessed: according to previous studies, correlations were considered strong for R2≥0.88. Results: The analysis included 269 3-month intervals of FGM data from 161 subjects (M/F=93/68; mean±SD: age 41±16 years, diabetes duration 21±14 years, insulin daily dose (IDD) 0.63±0.21 IU/kg, HbA1c 7.5±1.1%). The strength of correlations versus 90-day intervals increased with the duration of sampling periods (2, 4, 6, 8, 10 and 12-week intervals): only for TAR a relevant correlation versus 90-days data was almost found at 14 days (R2 0.87). For TIR and CV strong correlations were found for 4-week sampling periods (R2 0.89 for both), and for TBR no interval shorter than 6 weeks provided a similar strength (R2 0.87). When stratified for sex, age quartiles, HbA1c (> or ≤7.5%) and IDD (> or ≤0.6 IU/kg), for each time interval, TIR and TAR showed higher R2 values versus 90 days for males, lower HbA1c and lower IDD, while TBR and CV showed higher R2 values for higher IDD. Conclusion: These data suggest that the optimal number of days needed to provide an effective estimation of 90-day intervals of glucose metrics derived from FGM might depend not only on the specific metric being evaluated, but also on clinical characteristics of sensor users.