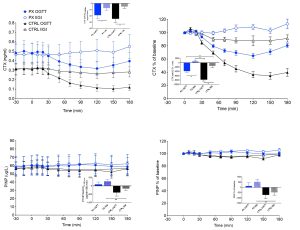
Background and aims: Gut hormones are recognised as pivotal in regulating postprandial bone turnover regulation in the so called “gut-bone axis”. However, disentangling the effects of gut stimulation on bone turnover from the well-established influences of glucose and pancreatic hormones (such as insulin, glucagon, and amylin) has proven challenging. Totally pancreatectomized (PX) patients serve as a unique model to elucidate the specific impact of gut stimulation on bone homeostasis independent of glucose and pancreatic hormones. The present study aims to investigate the acute effects of OGTT and isoglycaemic i.v. glucose infusion (IIGI) on bone resorption and formation markers in PX patients and healthy controls (CTRLs). Material and methods: Plasma samples from 10 PX patients (age: 59.8±9.9 years [mean±SD]; BMI: 21.5±4.3 kg/m2; HbA1c 67.3±11 mmol/mol) and 10 age-, sex- and BMI-matched CTRLs (age: 58.4±5.0 years; BMI: 22.9±2.4 kg/m2; HbA1c 34.6±6.2 mmol/mol) undergoing a 75 g-OGTT and corresponding IIGI on separate days were analysed for markers of bone resorption (C-terminal telopeptide of type 1 collagen [CTX]) and formation (procollagen type I N-terminal propeptide [PINP]). Results: Baseline plasma levels of CTX and PINP, respectively, were comparable in the two groups. Both groups exhibited significantly greater suppression of CTX during OGTT compared to during IIGI (Fig. 1). The PX patients exhibited significantly less maximal suppression of CTX levels during both OGTT (-35.5±3.3% vs -65.8±5.2% (mean±SEM), p<0.001) and IIGI (-0.7±0.1% vs -12±0.1%, p<0.001) compared to the CTRLs. PINP did not change significantly in response to OGTT or IIGI in any of the groups, but the PX patients displayed lower PINP maximal suppression compared to CTRLs (-6±1.4% vs -12.5±1.8%, p=0.011). Conclusion: Our findings support the existence of a gut-bone axis acting to reduce bone resorption in the postprandial state independently of prevailing plasma glucose and pancreatic hormone levels. Furthermore, the impaired glucose-induced suppression of CTX and PINP levels observed in PX patients could help to explain why these patients are prone to develop osteoporosis.