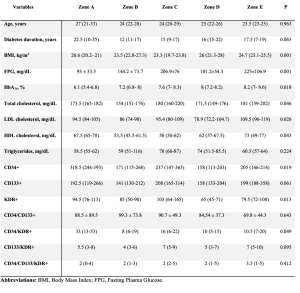
Background: Endothelial progenitor cells (EPCs) are involved in endothelial homeostasis and cardiovascular health. Both EPCs reduction and/or disfunction in people with type 1 diabetes (T1D) has been associated with poor glycemic control. The Glycemia Risk Index (GRI) is a novel composite metric, derived from continuous glucose monitoring (CGM) data, that describes the quality of glucose control according to the patients’ risk of hypoglycemia or hyperglycemia. Aim: 1) To evaluate the distribution of EPCs count in the GRI zones in a population of adults with T1D; 2) to investigate the relationship between the GRI and the other diabetes-related metrics with circulating levels of EPCs. Methods: This cross-sectional study included adults (>18 years) with T1D, treated with intensive insulin therapy and CGM use. GRI was calculated from CGM-derived metrics related to the 14 days prior the study visit. EPCs count was assessed by flow cytometry. EPCs count and GRI were described in the population stratified in five GRI zones, ranging from A (lowest risk) and E (highest risk). Results: Ninety-eight adults (median age 24.0 years) were included. Body mass index (BMI) (p=0.001), fasting plasma glucose (FPG) (p=0.001) and HbA1c values (p=0.018) were higher in participants with the worst GRI. Circulating levels of KDR+ and CD34/KDR+ cells were lower in participants with worse GRI in comparison with adults with better GRI. Results from univariate analysis showed that GRI was positively associated with FPG (rs=0.288, p=0.004) and HbA1c (rs=0.387, p<0.001). No significant association was found between GRI, EPCs count and other studied clinical variables. Conclusions: Adults with T1D with poor GRI showed lower CD34/KDR+ count. Further studies are needed to clarify the role of GRI for evaluating the cardiovascular risk of people with T1D.