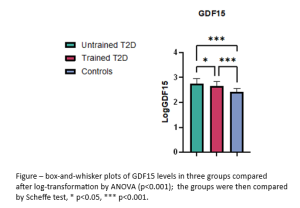
Fracture risk is increased in type 2 diabetes (T2D), independently of bone mineral density (BMD). Growth Differentiation Factor 15 (GDF15) is a senescence-associated secretory phenotype protein, increased in T2D. Exercise can reduce fracture risk, but is unknown whether it can alter GDF15 in T2D. This study was aimed at exploring the role of exercise training on GDF15 and musculoskeletal health in T2D.To this end, we performed a cross-sectional analysis of 118 T2D patients who participated in a 2-year intervention study and 48 non-diabetic controls. Of the T2D participants, 64 were from the combined exercise program group (trained) and 54 from the usual care control group (untrained); moreover, 15 had both baseline and end-of-study data. Age ranged from 65 to 75 years. Serum GDF15 was measured using an ELISA (R&D Systems). Other measures included: metabolic parameters, kidney function, bone measures (BMD, trabecular bone score -TBS-, bone turnover markers -BTMs-, calcaneal Quantitative UltraSound -QUS- and peripheric quantitative computed tomography -pQCT), physical performance (short physical performance battery -SPPB), physical fitness (expressed by VO2peak and metabolic equivalents, METs), muscle strength, mass and density. Physical activity (PA) level was assessed using questionnaires. GDF15 significantly differed among groups, with the highest levels in untrained T2D (figure; * p<0.05,*** p<0.001). Trained T2D had better muscle (but not bone) outcomes than untrained counterparts. In T2D, GDF15 was negatively associated with SPPB (ρ-0.18, p 0.05), VO2peak (ρ-0.25, p 0.005), METs (ρ-0.27, p 0.003), PA level (ρ-0.2, p 0.03), pQCT-derived muscle density (ρ-0.23, p 0.02), BMI (ρ -0.2, p 0.04), and eGFR (ρ-0.24, p 0.01). Multiple linear regression analysis revealed that SPPB (β-0.4, p<0.000), BMI (β-0.3, p 0.008), and eGFR (β-0.24,p 0.018) were independent determinants of GDF15 in T2D. Longitudinal analysis of 15 T2D participants showed significant GDF15 changes over the 2-year follow-up (Δ-415.6 pg/ml; p 0.03): GDF15 decreased by -155.7 pg/ml in trained T2D, with improvements in VO2, METs, SPPB and kidney function, while it increased by +260 pg/ml in untrained T2D.In conclusion, exercise training in T2D was associated with GDF15 reduction, supporting the hypothesis that exercise may counteract the ageing process in T2D and that GDF15 may mediate this response. GDF15 might influence fracture risk by exerting its actions on muscle (but not bone) function.