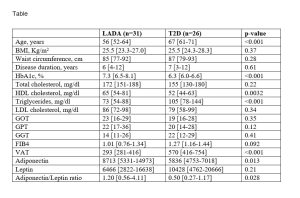
Background: Pathophysiology and complications of latent autoimmune diabetes in adults (LADA) differ from type 2 diabetes (T2D). Data about characteristics of liver disease in LADA are lacking. Aim: To compare liver steatosis and fibrosis between LADA and T2D. Methods. Liver magnetic resonance imaging (MRI) with elastography (MRE) were performed in 31 people with LADA and 26 with T2D, matched for sex, BMI and disease duration. Liver steatosis was defined for proton density fat fraction (PDFF) values >5.5%; augmented liver stiffness was defined for values ≥2.5 KPa. DXA was performed to evaluate body mass composition. C-peptide, adiponectin, and leptin levels were measured. Clinical and biochemical data were collected. Results: People with LADA were younger than those with T2D, with similar disease duration, BMI and waist circumference (Table). LADA had higher HbA1c, higher HDLc and lower triglycerides, with no differences in total cholesterol, LDLc, and liver enzymes. Despite the similar BMI, people with T2D were more frequently affected by liver steatosis (53.9% vs 6.5%, p=<0.001) and by augmented liver stiffness (44.0% vs 19.4%, p=0.046). Such differences were in part explained by the study of body mass composition and of adipokines, showing that people with LADA, had a lower amount of visceral adipose tissue (293 [281-416] g vs 570 [416-754], p<0.001) and higher adiponectin/leptin ratio (1.20 [0.56-4.11] vs 0.50 [0.27-1.17], p=0.028). Of note, augmented liver stiffness was very often associated with liver steatosis in people with T2D, but not in people with LADA (number of people with liver steatosis and augmented stiffness: 8/11 (72.7%) in T2D vs 0/6 (0%) in LADA, p=0.009). Among people with LADA, those with lower C-peptide values (<0.3 ng/ml) showed higher liver stiffness (2.3 [2.3-2.7] Kpa vs 2.1 [2-2.3], p=0.017). Conclusions: LADA subjects present a distinct liver phenotype compared to T2D, with significant differences in meta-inflammation and presence of augmented stiffness without steatosis. Lower C-peptide levels, likely reflecting greater pancreatic autoimmune load, were related with increased liver stiffness. These findings emphasize the importance of investigating liver involvement in LADA.