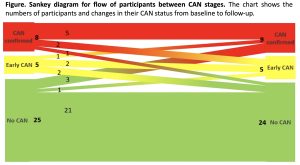
Objectives: This is a longitudinal retrospective study aimed at evaluating whether cardiovascular autonomic neuropathy (CAN) in type 1 diabetes (T1D) is reversible and the factors associated with change of CAN status. Methods: We evaluated retrospectively 38 participants with T1D (at baseline: age 39.1±13 years, diabetes duration 24.0±13 years, HbA1c 67±22 mmol/mol), followed for 4.9±1.98 years. We performed at baseline and follow-up 4 cardiovascular reflex tests (CARTs) and assessed clinical history and variables. We classified early and confirmed CAN in presence of 1 or 2 abnormal CARTs, respectively. CAN regression was defined as an improvement in CAN stage (from early to no CAN or from confirmed to early or no CAN) and CAN progression as the change from no CAN to early CAN or from early to confirmed CAN. Results: At baseline 5 (13.2%), 8 (21.05%), and 25 participants (65.8%) had early, confirmed and no CAN, respectively; at follow-up, 5, 9, and 24 participants had early, confirmed and no CAN, respectively, with one more participant with confirmed CAN (23.7%). In the whole population deep breathing test deteriorated significantly (p=0.03). At follow-up, CAN regression occurred in 5 (13.2%), CAN progression in 5 (13.2%), while CAN status was unchanged in 28 participants (Fig.). CAN progression was associated with higher body mass index (BMI) at baseline compared to the other groups (p<0.05) and at follow-up compared to CAN regression (27.6±2.01 vs 21.9±1.4 kg/m2, p<0.001), and with lower eGFR at follow-up compared with CAN unchanged (p=0.016). In a multivariate logistic regression analysis, including baseline BMI, age and sex, baseline BMI significantly predicted the risk of CAN progression [odds ratio 2.86 (95%CI 1.15-7.10), p<0.024]. Conclusions: In this well characterized population with T1D, we observed at 5-year follow-up an increase in overall CAN prevalence and a degree of CARTs deterioration lower than expected, with both progression and regression of CAN status. BMI seems to be the best predictor of CAN progression.