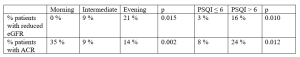
Background: Chronic complications of diabetes can be associated with sleep disorders concerning quality, quantity and chronotype. DKD is responsible for high mortality and low quality of life in diabetic people. The latest guidelines from ADA/EASD highlight that sleep is a central component in the management of T2DM, as well as other lifestyle-related behaviors. Aim: 1) To evaluate the chronotype and sleep quality in people with T2D and 2) to investigate the association with DKD. Methods: This retrospective study included 150 adults with T2D and regular follow-up in a tertiary-care center. Chronotype and sleep quality were assessed by administering the MEQ and PSQI, respectively. DKD was defined as the persistence of eGFR<60 mL/min/1.73 m2 and/or ACR ≥30 mg/g. According to MEQ, the study cohort was stratified in 3 chronotypes: morning (23%), intermediate (58%) and evening (19%). According to PSQI, 2 groups were identified: poor sleepers (49%) and good sleepers (51%). Results: The intermediate chronotype was significantly prevalent in this study population (p=0.018). The proportions of patients with reduced eGFR or with ACR in morning, intermediate and evening chronotypes were 0%, 9% and 21% (p=0.015) and 35%, 9% and 14% (p=0.002), respectively. Compared with good sleepers, poor sleepers were associated with higher levels of ACR (8% vs 24%, p=0.012) and reduced eGFR (3% vs 16%, p=0.01) (Tab. 1). Conclusions: In this real-world experience of people with T2D, the intermediate chronotype is more frequent than morning and evening chronotypes. Moreover T2D patients with evening chronotype and lower sleep quality showed worse renal function.