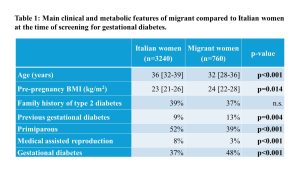
Background: Over the past decade, migration flows have brought many women of childbearing age to Italy, some with high-risk ethnicity for gestational diabetes (GDM). However, the extent of migration and its impact on the prevalence and outcomes of GDM in Italy are little known. Methods: In this single-center, retrospective, observational study, we evaluated pregnant women who performed the screening for GDM in our Diabetes Unit between 2012 and 2022. The prevalence of GDM was compared between Italian and migrant women. In GDM women, metabolic features during pregnancy and neonatal outcomes (preterm, large and small for gestational age) were also assessed. Results: Clinical and metabolic data of 4000 pregnant women (81% Italian, 19% non-Italian) were evaluated. The proportion of migrant pregnant women significantly increased, from 5% in 2012 to 25% in 2022 (p<0,001). In 2022, migrant women mainly were from Albania (18%), Bangladesh (13%), Morocco (12%), Philippines (11%), and Romania (11%). Italian women were older, and more frequently at their first pregnancy, compared to migrant women. Moreover, medical assisted reproduction was more common in Italian women, while non-Italian women had higher pre-gestational BMI and more frequently a history of GDM. The prevalence of GDM was higher in non-Italian women (Tab. 1). In GDM women, metabolic control during pregnancy was worse in migrants (3rd trimester HbA1c 5.3 [5.1-5.6] vs 5.2 [5.0-5.4]%, p<0.001) and, despite similar gestational weight gain (10 [7-13] kg in migrants and 11 [9-14] kg in Italian) and proportion of women treated with insulin (26% in both groups), non-Italian women more frequently required pre-prandial insulin therapy (34% vs 21%, p=0.007), either alone or in combination with basal insulin. Neonatal outcomes were comparable between the two groups. Conclusions: Over the past 10 years, the percentage of non-Italian pregnant women referred to our Clinic increased five-fold and, nowadays, one in four women is not Italian. The prevalence of GDM was higher in migrant women, and migrant women with GDM had worse metabolic control during pregnancy and more frequently required pre-prandial insulin therapy. More intensive treatment, close monitoring, management by a multidisciplinary team and free access to healthcare services may explain similar neonatal outcomes in the two groups.