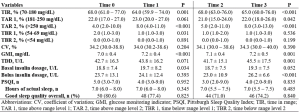
Context: There is a bidirectional relationship between the management of type 1 diabetes (T1D) and sleep quality and timing. Aim: To investigate the sleep quality and the glucose metrics in people with T1D at the seasonal clock adjustment. Methods. This observational study involved adults with T1D, treated with multiple daily insulin injections with continuous glucose monitoring (CGM) or Hybrid Closed Loop, who completed the Pittsburgh Sleep Quality Index questionnaire. We compared the CGM-derived metrics and sleep quality observed before (Time 0) and after (Time 1) transition in autumn and before (Time 2) and after (Time 3) transition in spring. Main Outcome Measure(s). Change in glucose monitoring indicator (GMI), time in range (TIR), time above range (TAR) and time below range (TBR). Results: Sixty-two participants (median age 26 years) showed no changes in sleep quality at time transitions. The values of GMI increased during both time transitions [Time 0 vs Time 1, 7.0 (6.7-7.2) vs 7.2 (6.9-7.4), %, p<0.001; Time 2 vs Time 3, 7.0 (6.8-7.4) vs 7.2 (6.8-7.5), p=0.006]. The percentage of TIR decreased from Time 0 to Time 1 (p<0.001) and from Time 2 to Time 3 (p<0.001). The percentage of level 2 TAR significantly increased during the observation (Time 0 vs Time 1, p<0.001; Time 2 vs Time 3, p<0.001). Conclusions: At similar level of sleep quality, adults with T1D underwent the worsening of most of CGM-derived glucose control metrics during the transition time.