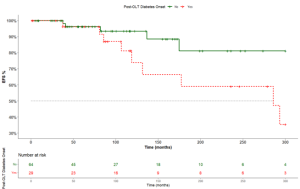
Background: Orthotopic liver transplantation (OLT), a critical intervention for end-stage liver disease, has shown substantial short-term survival progress. However, despite advancements, cardiovascular events remain a significant cause of long-term post-transplant morbidity and mortality. The aim of this study is to assess the occurrence of long-term cardiovascular events and whether it relates to new-onset diabetes after liver transplantation (NODALT). Methods: We conducted an observational multicentric retrospective analysis of adult OLT recipients with regular follow-up visits up to six months from January 1995 to December 2020. The minimum follow-up period was two years post-intervention. Anamnestic, clinical, anthropometric, and laboratory data were collected across two centres. NODALT was diagnosed based on the ADA guidelines (HbA1c and/or plasma glucose criteria). The primary outcome was an incident cardiovascular event (CVE, defined as a composite of fatal and non-fatal stroke and myocardial infarction). CVE was recorded and analyzed in relation to the NODALT diagnosis. Furthermore, clinical characteristics associated with the development of NODALT were analyzed. Results: Ninety-three eligible Caucasian patients, with a median age of 57 years (IQR: 49.0-62.0, 69.9% male), were enrolled. Over the median follow-up period of 100.5 months, 29 patients (31.2%) developed NODALT and 14 patients (15.1%) developed any CVE, with 9 being in the NODALT group. A significant association between NODALT and cardiovascular complications was confirmed by both generalized estimating equation (OR 5.31; 95%CI 1.59-17.72, p=0.006) and Kaplan-Meier analysis (log-rank=0.046). Metabolic syndrome and impaired fasting glucose were identified as baseline risk factors for the incident NODALT (OR 5.75; 95%CI 1.44-22.92, p=0.013 and OR 7.29; 95%CI 1.46-36.41, p=0.015, respectively). Conclusions: Post-OLT cardiovascular events occur less frequently than previously reported, but they are notably linked to NODALT, underlining the interplay between metabolic syndrome and impaired fasting glucose. These insights could provide a foundation for targeted preventive strategies and enhanced post-transplant management.