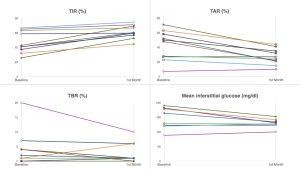
Background and aims: Total pancreatectomy (TP) patients exhibit absolute insulin deficiency because of the removal of the entire β-cell mass. Moreover, TP results in alterations in gastrointestinal anatomy, coupled with the loss of other pancreatic peptides such as glucagon and amylin. As a result, these patients show high insulin sensitivity and elevated glycemic variability when treated with multiple daily insulin injections. In addition, it is common for TP patients to be of advanced age and experience difficulties in using diabetes technology. This observational study aimed to gather data on CGM metrics in TP patients who switched from multiple daily insulin injections (MDI) to insulin pumps. Methods: Observational study of 13 TP patients. Following surgery, all patients underwent initial treatment with MDI and either used continuous glucose monitoring (CGM) or self-monitoring of blood glucose. Patients received training in carbohydrate counting or were provided with simplified tables for carbohydrate counting (small-medium-large meals based on food diaries). CGM metrics were collected before and after switching to an insulin pump. Four patients also completed quality of life questionnaires before and after pump use. Results: After a median of 20.8 months (range 0.1-143.3), they were switched to an insulin pump. Median age was 65 years (range 55 to 77). 4 patients used a continuous subcutaneous insulin infusion pump (CSII) and an intermittent-scanning CGM (is-CGM) for glucose monitoring, while the other 9 patients used a and advanced hybrid closed loop system (AHCL) with the appropriate real-time CGM (rt-CGM). In the first month of insulin pump use, compared to the 30 days before switching to the insulin pump, we observed an increase in time in range (TIR; from 53.2% to 69.2%, p=0.005), and a decrease in time above range (TAR; from 42.7% to 27.1%, p=0.011), without a significant increase in time spent in hypoglycemia (from 4.1% to 2.7%, p=0.228). Prior to using the insulin pump, the median level of HbA1c was 7.73% (range 6.1% to 9.9%), while GMI during the initial month of pump usage was 6.8%. When analyzing CSII and AHCL patients separately, the improvement remained significant only in those who were switched to an AHCL. Quality of life improved with AHCL use. Conclusions: Our preliminary data indicate that AHCL enhances glycemic control and improves quality of life in patients undergoing total pancreatectomy.